please start at question 13 and answer the following ones13-28.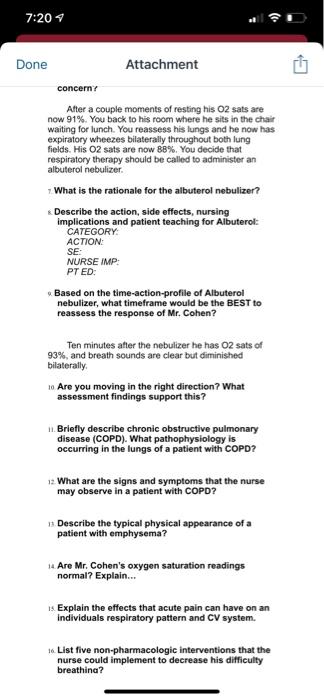
7:20 Done Attachment concerny After a couple moments of resting his O2 sats are now 91%. You back to his room where he sits in the chair waiting for lunch. You reassess his lungs and he now has expiratory wheezes bilaterally throughout both lung fields. His O2 sats are now 88%. You decide that respiratory therapy should be called to administer an albuterol nebulizer What is the rationale for the albuterol nebulizer? Describe the action, side effects, nursing implications and patient teaching for Albuterol: CATEGORY: ACTION: SE: NURSE IMP: PT ED . Based on the time-action-profile of Albuterol nebulizer, what timeframe would be the BEST to reassess the response of Mr. Cohen? Ten minutes after the nebulizer he has 02 sats of 93%, and breath sounds are clear but diminished bilaterally 10 Are you moving in the right direction? What assessment findings support this? 1. Briefly describe chronic obstructive pulmonary disease (COPD). What pathophysiology is occurring in the lungs of a patient with COPD? 12. What are the signs and symptoms that the nurse may observe in a patient with COPD? 13 Describe the typical physical appearance of a patient with emphysema? 1. Are Mr. Cohen's oxygen saturation readings normal? Explain... 1s Explain the effects that acute pain can have on an individuals respiratory pattern and CV system. 16 List five non-pharmacologic interventions that the nurse could implement to decrease his difficulty breathing?
7:20 Done Attachment 17 How could you measure the effectiveness of the interventions listed above? ik Explain why it is not best practice to increase his oxygen to help ease his SOB when he was at the nurses' station? 14. What are three non-pharmacologic nursing interventions to help manage his pain? 20. How would you measure the effectiveness of the interventions to manage pain without drugs? 21. Should you be concerned with the adverse effects of respiratory depression and hypotension when giving Percocet? Why or why not? 22. What are three nursing diagnostic priority statements that reflect Mr. Cohen's current status? For each statement list 3 interventions with rationale. Statement Statement: Statement You finally receive the following lab results that were ordered upon admission: Basic Metabolic panel: BUN: 32 Creatinine 1.42 Sodium: 138 Potassium: 3.2 Calcium: 9.5 Glucose: 165 GFR-45cc/minute CBC: : WBC: 14.0 Neutrophils: 88% Bands: 11% Lymphocytes 12% Hgb: 13,3 Pit: 217 CXR: Large bilat lower lobe infiltrates
7:20 Done Attachment 23. Identify the lab results above that are elevated/abnormal and their clinical significance: 2. What is the most likely cause of Mr. Cohen's exacerbation of his respiratory status? What will you specifically assess more closely and what will change in your initial plan of care based on this lab findings? You need to reconcile and verify Mr. Cohen's home medications. As you do this, state the reason he is taking each medication based on its indication and its mechanism of action: > Home Medications Advair (fluticasone & salmeterol) diskus 1 puff every 12 hours INDICATION: ACTION Albuterol MDI 1-2 puffs every 4 hours prn INDICATION: ACTION: Lisinopril 10 mg po daily INDICATION: ACTION: Triamterene-HCTZ 1 tab daily INDICATION ACTION: Valium 2.5 mg po every 6 hours as needed INDICATION: ACTION: Gemfribrozil 600 mg po bid INDICATION: ACTION: Metformin 500 mg po bid INDICATION: ACTION z Mr. Cohen will be returning home with oxygen after discharge. List at 3-5 safety considerations you should include in your discharge teaching regarding the use of home oxygen.
7:21 Done Attachment Home Medications Advair (fluticasone & salmeterol) diskus 1 puff every 12 hours INDICATION: ACTION: Albuterol MDI 1-2 puffs every 4 hours prn INDICATION: ACTION Lisinopril 10 mg po daily INDICATION: ACTION: Triamterene-HCTZ 1 tab daily INDICATION: ACTION: Valium 2.5 mg po every 6 hours as needed INDICATION: ACTION: Gemfribrozil 600 mg po bid INDICATION: ACTION: Metformin 500 mg po bid INDICATION: ACTION 27 Mr. Cohen will be returning home with oxygen after discharge. List at 3-5 safety considerations you should include in your discharge teaching regarding the use of home oxygen. What is "pursed lip breathing" and how does it help improve the ventilation of those with COPD? Be sure to include this in your teaching plant
没有找到相关结果