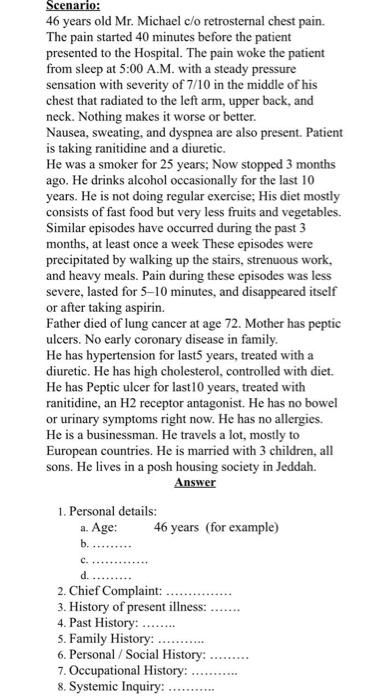
Scenario: 46 years old Mr. Michael c/o retrosternal chest pain. The pain started 40 minutes before the patient presented to the Hospital. The pain woke the patient from sleep at 5:00 A.M. with a steady pressure sensation with severity of 7/10 in the middle of his chest that radiated to the left arm, upper back, and neck. Nothing makes it worse or better. Nausea, sweating, and dyspnea are also present. Patient is taking ranitidine and a diuretic. He was a smoker for 25 years; Now stopped 3 months ago. He drinks alcohol occasionally for the last 10 years. He is not doing regular exercise; His diet mostly consists of fast food but very less fruits and vegetables. Similar episodes have occurred during the past 3 months, at least once a week These episodes were precipitated by walking up the stairs, strenuous work, and heavy meals. Pain during these episodes was less severe, lasted for 5-10 minutes, and disappeared itself or after taking aspirin. Father died of lung cancer at age 72. Mother has peptic ulcers. No early coronary disease in family. He has hypertension for last5 years, treated with a diuretic. He has high cholesterol, controlled with diet. He has Peptic ulcer for last 10 years, treated with ranitidine, an H2 receptor antagonist. He has no bowel or urinary symptoms right now. He has no allergies. He is a businessman. He travels a lot, mostly to European countries. He is married with 3 children, all sons. He lives in a posh housing society in Jeddah. Answer 1. Personal details: a. Age: 46 years (for example) b. c. d. 2. Chief Complaint: 3. History of present illness: 4. Past History: 5. Family History: 6. Personal / Social History: 7. Occupational History: 8. Systemic Inquiry:
没有找到相关结果